The Common Vein Copyright 2010
Introduction
Size and the Menstrual Cycle
The cyclical changes of the menstrual cycle present a continual change of events controlled by a series of integrated hormonal events. These changes are most easily observed in the endometrium by ultrasound. During the menses, the endometrium sheds and becomes thinner, the junctional zone is irregulalrly thick, and the myometrium loses water and thins.
During the menstrual phase (days 1- 4) the the endometrium is thin and typically is seen as a single echogenic line by ultrasound examination, and measuring between 1-4mm thick reflecting the early development of glands and stroma.(Nalaboff)
During the proliferative phase (days 4-14) the endometrium is of intermediate thickness. In the early phase as the glands, stroma and vessels start to regenerate the stripe is echogenic and slightly thicker measuring and measures between 5-7mms thick by ultrasound. Later as the the tissue matures in the preovulatory phase the stripe has a typical trilaminar appearance and thickness measures up to 11mms. (Nalaboff)
During the secretory phase (days 15-28) the endometrium is at its thickest in midsecretory phase and has a typical homogeneously echogenic appearance. It usually measures between 7-16mms. (Nalaboff)
Changes in the Endometrial Stripe
During the menstrual cycle the ultrasound appearance can characterise and date the phase of the cycle. (Nalaboff) Following menses there is a thin echogenic line which measures between 1-4mms, (Nalaboff) which progressively thickens and changes to a multilayered configuration. On ultrasound the measurement is from echogenic border to echogenic border in the sagittal plane.
|
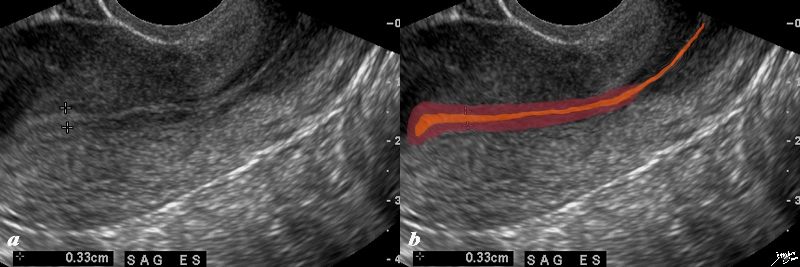
First Week Post Menstruation Early Proliferative Phase |
|
The normal sagittal view of the uterus is a transvaginal ultrasound, in the first week after menstruation after menstruation, and just prior to the next menstruation after the endometrium has been shed. It demonstrates that the endometrium becomes a single echogenic line consisting of opposing walls (orange) and is surrounded by a subendometrial halo of the junctional zone (tan). This layer is more compacted, and relatively hypovascular. This image is typical of the early proliferative phase. It is during this time that estrogen starts to rise and progesterone has fallen. The endometrium in this case measures about 3mms Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 84698c02b.8s |
In the proliferative phase (day6-14) the endometrium thickens to 5-7mmsand becomes more echogenic than the myometrium.This reflects growth of the endometrial glands blood vessels and stroma, stimulated by estrogen production by the ovarian follicles. This proliferative endometrium is structurally and functionallly prepared for implantation of the fertilised egg. In the late proliferative phase (periovulatory phase), the endometrium becomes multilayered, with an echogenic basal layer, hypoechoic inner functional layer and a thin echogenic line
|
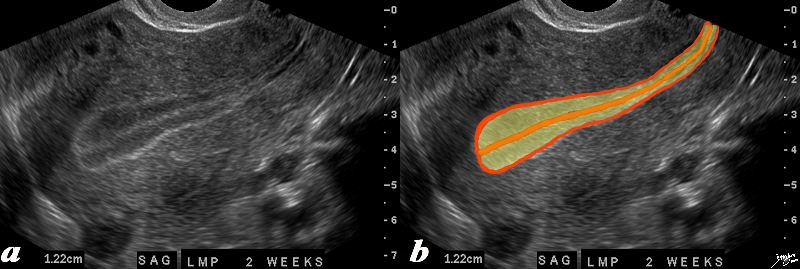
Trilaminar Appearance – Midcycle Preovulation End of Proliferative Phase |
|
The normal sagittal view of the uterus is a transvaginal ultrasound, 2 weeks after menstruation, and just prior to ovulation. It demonstrates that the uterus and more specifically the endometrium is more complex than just a simple columnar epithelium. This is an example of the trilaminar appearance of the endometrium and is characteristic of the appearance of the endometrium in the preovulatory phase. This pahse is also called the follicular phase, or proliferative phase. It is during this time that estrogen is the dominant hormonal influence. The appearance is also known as a “triple stripe”, and conversely, its presence is seen before progesterone is produced. If present with a 9mm+ diameter, it reflects an ideal potential lining for fertilization.. In this case it measured 1.2cms. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 83835c02.8s |
Following ovulation, the endometrium is under the influence of progesterone secretion by the corpus luteum. The endometrial glands fill up with mucus. The resulting appearance of the endometrium is a thick echogenic structure (secretory phase) The endometrium is at its thickest at this stage (< 14mm). As luteinizing hormone levels fall in the latter phase of the cycle, the level of progesterone falls, and there is shedding of the endometrium. Thus, the cyclical changes of the endometrium (invisible, thin echogenic, multi-layered, thick echogenic) reflect the phases of the menstrual cycle. “Transvaginal ultrasound revealing an endometrial stripe of less than 5 mm is reassuring and essentially rules out cancer (3). An endometrial stripe greater than 4 mm necessitates endometrial sampling, preferably with in-office use of a Pipelle endometrial suction curette or similar device”
In the periovulatory phase the myometrium and endometrium start to thicken, and the junctional zone becomes more easily identified (Kido)
There are 3 distinct zones or parts of the uterus which vary in size and character during each of the menstrual phases.
Endometrial Changes During the Cycle
During the follicular phase (proliferative phase) which occurs in the first half of the cycle, and after the shedding of the endometrial lining, there is a rise in estrogen which causes the endometrial lining to start to thicken. In mid cycle after ovulation, luteinizing hormone is released, which heralds in the luteal phase (aka secretory phase). Progesterone now rises and further proliferation of the endometrium occurs. In the absence of pregnancy progesterone levels and estrogen levels fall, and the endometrium sheds. The cervical canal has a maximal dimension of 8mms.
|
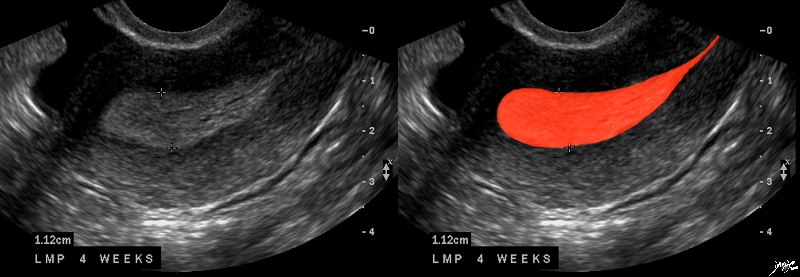
Premenstrual Endometrium End of Secretory Phase |
|
The normal sagittal view of the uterus is a transvaginal ultrasound, about 4 weeks after menstruation, and just prior to the next menstrauation when the endometrium is overripe. It demonstrates that the uterus and more specifically the endometrium is more complex than just a simple columnar epithelium. This is an example of the hyperechoic, homogeneous, thick endometrium characteristic of the secretory phase. It is during this time that progesterone is the dominant hormonal influence and estrogen influence is minimal. The endometrium in this case measures 1.2cms. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 46318c01.8s |
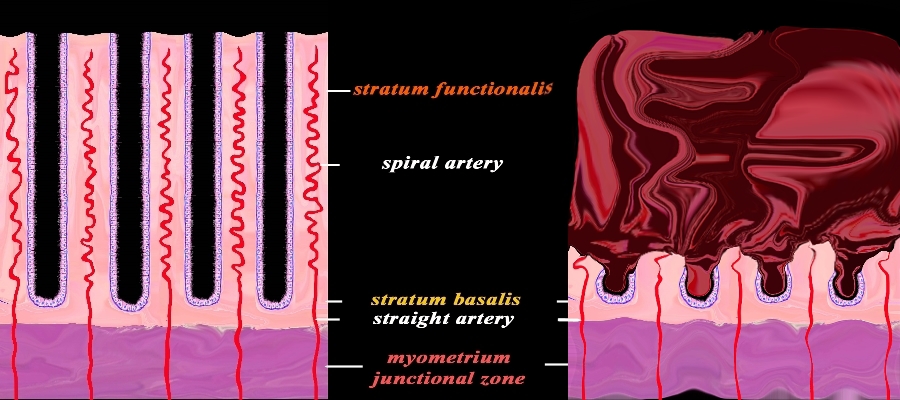
Menstruation |
|
The diagram reflects the premenstrual endometrium (left) and the post menstrual endometrium right, revealing the necrosis of the functional layer with sloughing and hemorrhage. The basal layer with the staright arteries and a small portion of the spiral artery remains intact. The hemorrhage is controlled by spasm of the arteries and contraction of the myometrium. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 32347f08cL.92s |
Myometrial Changes
The myometrium is largest in the second half of the cycle – the midsecretory phase. The myometrium is thickest at this time due to mild edema, but this is not easily observed by imaging techniques.
Junctional Zone Changes
During the midsecretory phase the junctional zone thins out.
In the post menopausal woman the average size of the uterus is 5cms in craniocaudad span by 2cms.(Fleischer )
In virgin state the uterus is flattened antero-posteriorly and is pyriform in shape, with the apex directed downward and backward. The bladder is to anterior and rectum is related to it posteriorly. It is a pelvic organ suspended by broad ligament and round ligament superiorly to pelvic fibrous tissue inferiorly.
The Post Menopausal Uterus
The postmenopausal uterus should measure about 3.5 – 7.5cms in c-c span by 1.7-3.3cms in A-P by 2-4 cms in transverse.
|
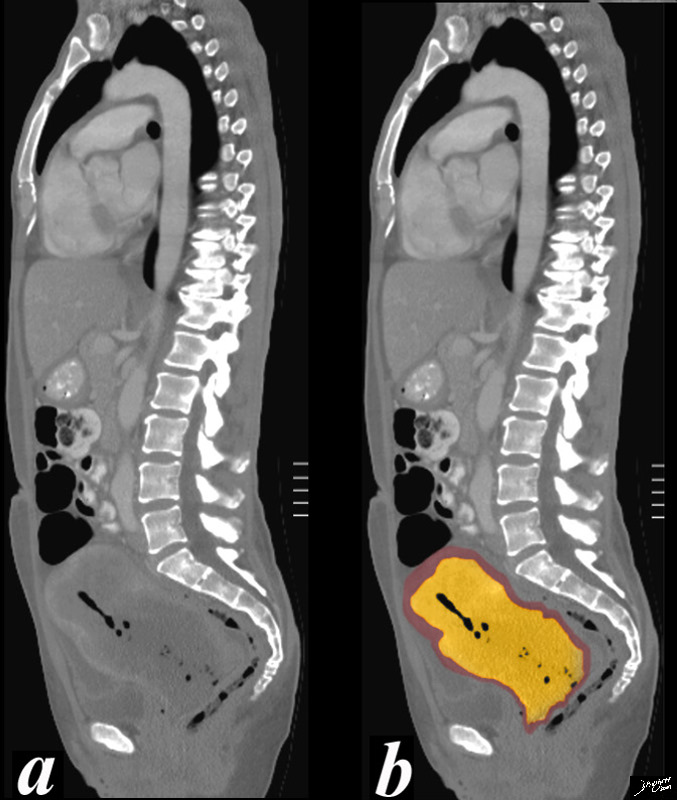
The Small Uterus Age Related Involution |
|
86 year old female with a small but age appropraiate sized uterus measuring only about 3.5cms in length and 2cms in A-P dimension. She presented with back pain and the sagital reformatted CT shows a grade 1 spondylolisthesis of L5 on S1 with discogenic disease. Courtesy Ashley Davidoff MD Copyright 2010 75922c03 |
|
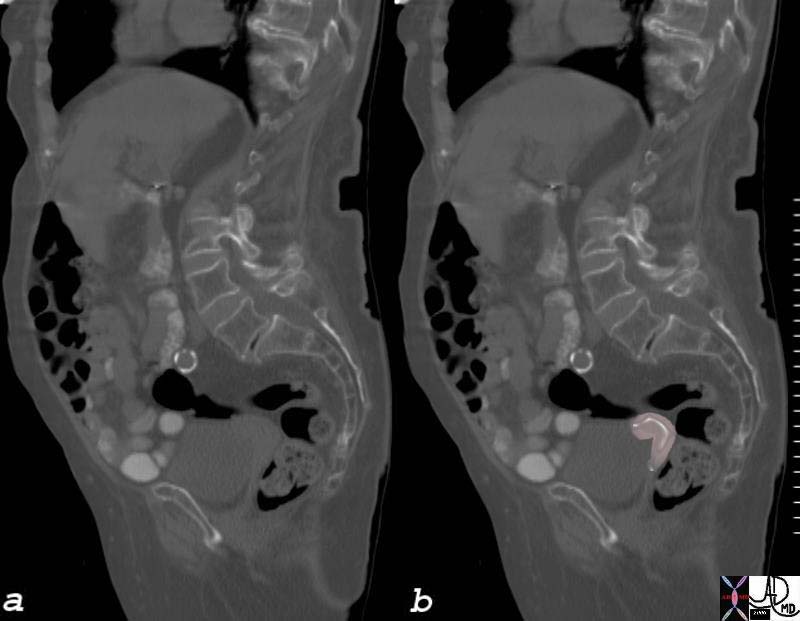
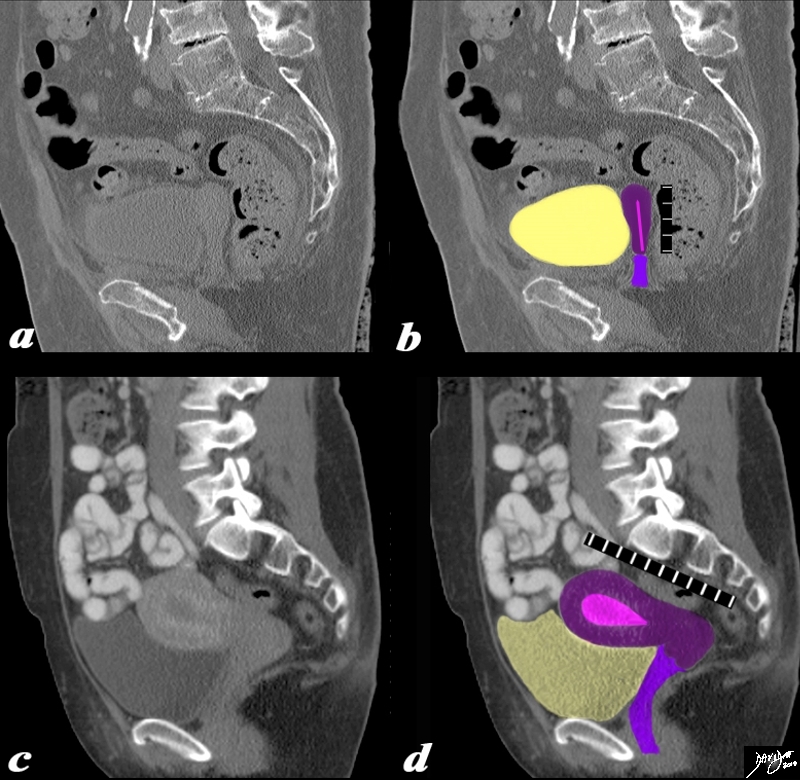
Age Related Involutional Changes (a,b) and Normal (c,d) |
|
The sagittaly reconstructed CT of a 82 year old female (a,b) is placed in comparison to a similar view in an 25 year old female (c,d),and size change is the most obvious difference. In the older patient the craniocaudad span (c-c) is about 5cms and A-P dimension is 1.5cms, and in the younger patient it is about 9cms in c-c span and 4.5cms in A-P dimension. The endometrial stripe in the older patient is not really visible but is drawn in a s a less than 1mms line and in the younger patient it is obvious and measures about a 1cms. In both instances the uterus is buoyed and cushioned by partly filled bladder (yellow) Note also the difference in the density of the bones, the degenerative changes in the spine and the calcification in the older patient of the distal abdominal aorta. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 83564c03.8s |
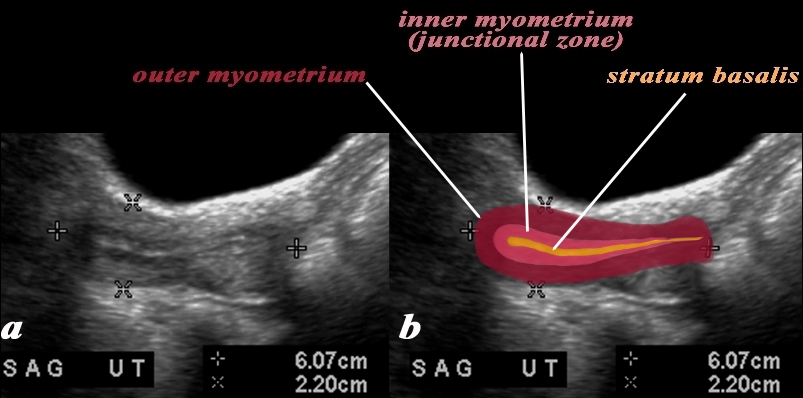
Post Menopausal Uterus |
|
In this 60 year old female with normal atrophied post menopausal uterus the transabdominal ultrasound in the sagittal plane reveals a normal view of the uterus with characteristic postmenopausal appearance. The stripe is thin measuring about 2mm homogeneously echogenic but also shows a hypoechoic halo of the junctional zone or inner myometrium. (salmon) The echogenic stripe is made up from a single histological layer the stratum basalis (deep yellow) The next layer as stated above is the compact myometrium – the junctional zone (aka inner myometrium) , and is followed by the thicker outer myometrium (maroon). Courtesy Ashley Davidoff MD Copyright 2009 all rights reserved 83573c01.81L |
|
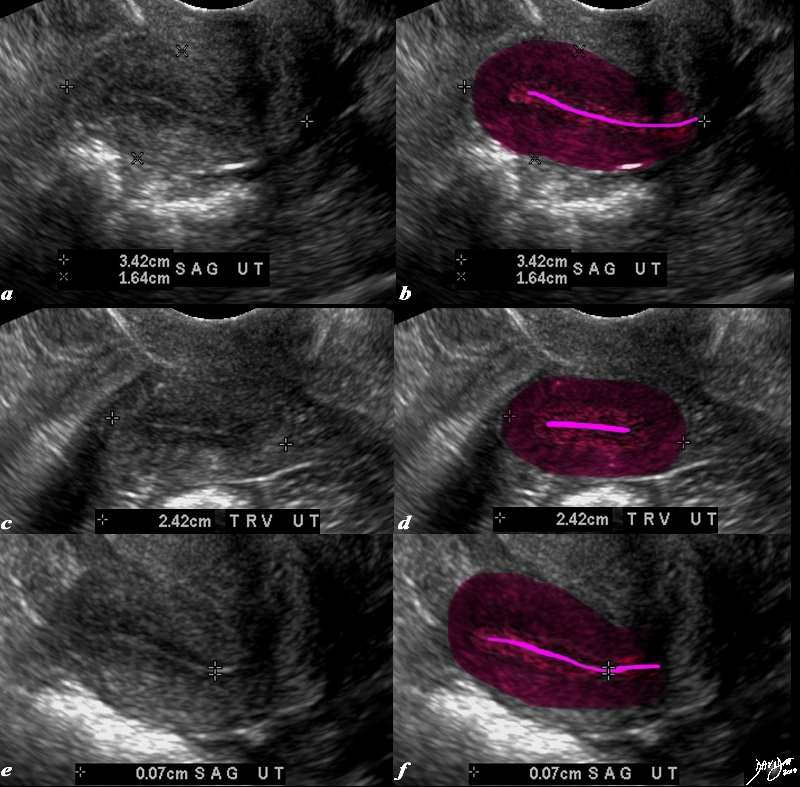
Endometrial Stripe in the Post Menopausal Uterus |
|
The transvaginal ultrasound is from a 62 year old post menopausal patient who presents with pelvic discomfort. The ultrasound shows a small atrophied uterus. The myometrium (dark red) junctional zone (light red) and endometrial cavity (pink) are outlined. In the sagittal plane the uterus measures 3.4cms in cranoicaudal dimension by 2.4cms in anteroposterior dimension (a,b) In the axial dimension (c,d) the uterus measures 2.4cms. The endometrial stripe is measured in the sagittal plane and measures .7mms. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 84711c01.8s |
|
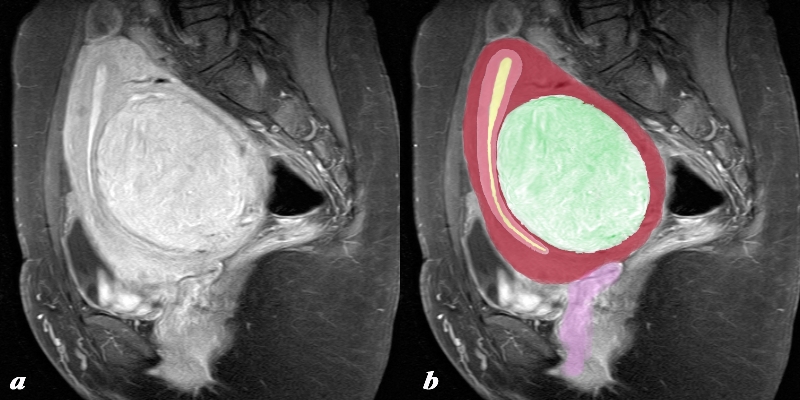
Single Large Fibroid Causing Uterine Enlargement |
|
The sagittal SPIR sequence from an MRI study shows a single large fibroid situated in the body of the uterus (green) and displacing and enlarging the remaining uterus forward and upward. The endometrial cavity is compressed (yellow) as is the junctional zone (salmon red) and the myometrium itself (maroon) The uterus has been lifted out of the pelvis and could be palpated clinically. The morphology of the swirling like shape to the myocardial tissue – an exemplary finding under the microscope is well appreciated in this image Courtesy Philips Medical Systems Images rendered by Ashley Davidoff MD Copyright 2010 All rights reserved 96932c01.8s |
|
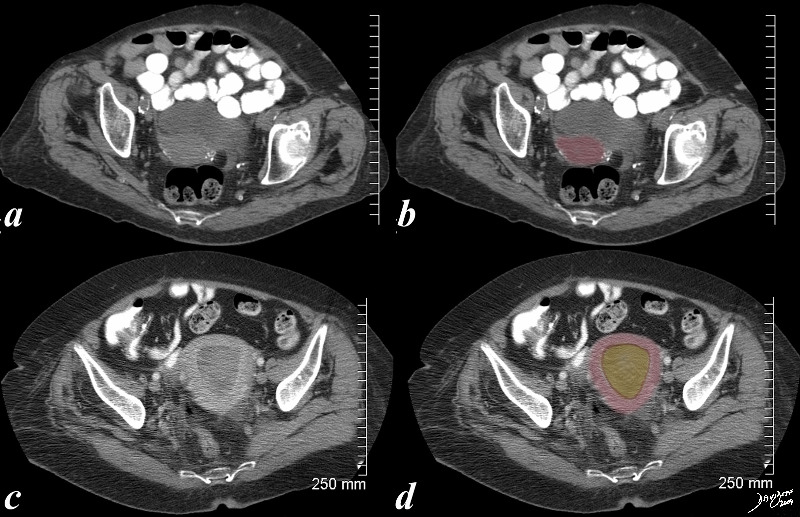
Normal Senescent Uterus and Uterine Carcinoma |
| The first CTscan (a,b) is from an 86 year old patient with a small but normal post menopausal uterus showing characteristic vascular calcification. The second CT (c,d) is from an 83F year old patient with distended endometrial cavity (orange in d) uterine carcinoma
Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 83731c01.8S |
|
Cervical Carcinma and Obstruction |
|
46 year old female with obstructed uterus and fluid filled endometrial cavity with pockets of air caused by cervical carcinoma complicated by pyometria Courtesy Ashley Davidoff MD Copyright 2009 all rights reserved 83682c01b.8s |
References
Fleischer AC, Kepple DM. Normal pelvic anatomy as depicted by various sonographic techniques. In: Fleischer AC, Javitt MC, Jeffrey RB, Jones HW, III, eds. Clinical gynecologic imaging. Philadelphia, Pa: Lippincott-Raven, 1997; 10-41.
(Kido)
Nalaboff, Kenneth M. MD, Pellerito, John S. MD and Ben-Levi, Eran MD Imaging the Endometrium: Disease and Normal Variants RadioGraphics, 21, 1409-1424. November 2001