The Common Vein Copyright 2008
Barry Giglio MD
Definition
Ectopic Pregnancy is a disorder where a gestation is located in a location other than the uterus, most commonly in a fallopian tube, but can occur on an ovary or intra-abdominally. It is characterized by pelvic pain associated with vaginal bleeding and a positive pregnancy test. Predisposing factors include previous ectopic pregnancy, pelvic infections (such as Pelvic Inflammatory Disease (PID)). Ectopic Pregnancy can result in serious complications including hemodynamic instability and death. Diagnosisis suspected clinically by a positive pregnancy test, pelvic pain, and/or vaginal bleeding. It is confirmed by characteristic changes in the velocity of Beta-HCG and ultrasound findings. Treatment options depend on whether the patient is hemodynamically stable, but include expectant management, medical and surgical management.
Principles
The principles revolve around the malpositioning of the fertilized ovum. The fertilized ovum has to be in the correct space to develop to full term. Once fertilization takes place, division starts immediately and the in the early stages the process can continue anywhere in the pelvic cavity requiring any space with minimal blood supply for this to occur. As the developing fetus evolves it requires additional nutrition and the evolving placenta requires the fertile and vascular endometrium to continue to full development. In the ectopic situation this is not available and the developing embryo will continue to seek new blood supply. In the rare situation where the pregnancy is intraabdominal it will find this nutrition in the mesenteries of the abdomen and will implant there until the catrastrophic situation where an advanced pregnacy may precitate a catastrophic bleed. The more usual situation of a tubal ectopic pregnancy can be dramatic but will present earlier. Thus the most basic principle relates to the position and space that is essential to full development. The fertilized ovum can only develop to full term in the endometrial cavity.
Structural Principles
The uterus is uniquely structured to accommodate, nourish, and protect a growing pregnancy. Other structures in the pelvis and abdomen are unable to accommodate or support a pregnancy and an ectopic can lead to serious life threatening consequences. The developing placenta “invades” the endometrial lining which becomes primed for the invasion, to set up a transport and filtering mechanism so that maternal blood rich in nutrients can transfer this blood to the fetus, and can also receive the fetal blood to export waste for the fetus.
| The Normal Fallopian Tubes |
| 46376 4376b01b01b03 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity |
| The Normal female System |
| 46376b11 pelvis uterus Fallopian tubes fimbrae uterus uterine cavity |
Physiological Principles
Pregnancy occurs after an egg is released from an ovary and is then taken up by the fimbria of the fallopian tube and fertilized with sperm. Normally, it is then transported through the fallopian tube to the uterus. The uterus is uniquely able to accommodate and support the growing gestation. The uterus is able to expand, supply to necessary blood supply via implantation into the endometrium, and provide a protective environment in amniotic fluid.
Principles of Disease
The
Cause and Predisposing Factors
Cause and Predisposing Factors: There are multiple predisposing factors, including those which alter the structure and function of the fallopian tubes. These include previous ectopic pregnancy or fallopian tubal surgery, PID. Other factors include cigarette smoking, use of fertility drugs and previous use of some intrauterine devices, and of course being a female of child bearing age. For unclear reasons, females over the age of 35 are also at higher risk for ectopic pregnancy.
Pathophysiology and Pathogenesis
Pathophysiology and Pathogenesis: The most common location of an ectopic pregnancy is in a Fallopian Tube, most commonly in the ampullary portion. The abnormally implanted gestation draws its blood supply from the organ within which it is implanted. Symptoms of an ectopic pregnancy typically start at approximate week number seven of a pregnancy, when the gestation is becomes too large for the organ within which it is implanted to accommodate. This can lead to rupture of the organ, uncontrolled bleeding and even death.
Result
Potential Complications
As noted above, with one episode of ectopic pregnancy, the risk of another episode increases. Other potential complications include affected future fertility due to scarring. Ultimately, this condition may lead to hemorrhage and death.
Diagnosis
The diagnosis of ectopic pregnancy involves a complex but standardized approach. This involves a careful history and physical examination and a high index of suspicion along with appropriate laboratory studies and imaging.
Clinical
The classic presentation of ectopic pregnancy includes amenorrhea (no periods for more than 6-7 weeks), pelvic pain, and vaginal bleeding. Many patients do not have this classic presentation, however. Anytime a woman presents with pelvic or abdominal pain associated with amenorrhea, one must consider ectopic pregnancy. A positive pregnancy test along with a normal or slightly enlarged, often tender uterus or adnexal mass is highly suggestive of ectopic pregnancy. However, no combination of physical findings can definitively diagnose an ectopic pregnancy.
Differential Diagnosis
Includes multiple conditions which can cause acute pelvic pain including Pelvic Inflammatory Disease (PID), spontaneous abortion (SAB), appendicitis, and kidney stones. In pelvic inflammatory disease, kidney stones, and appendicitis, pregnancy testing is typically negative and vaginal bleeding is less likely. Perhaps most difficult to differentiate are spontaneous abortions from ectopics. On physical exam, there may be pregnancy tissue present in the os in a spontaneous abortion which is typically not the case with an ectopic pregnancy. Also, the ultrasound findings may be different and the serum HCG level typically falls more quickly with an SAB.
Lab Tests
A laboratory evaluation should include a quantitative serum human chorionic gonadotropin (HCG) level, complete blood count, along with kidney and liver function. In a normal pregnancy, the HCG level typically will double every 48 hours in early pregnancy but will not in ectopic pregnancy. Typically, the HCG will go do down in SAB. Sometimes, a serum progesterone level can also be helpful in determining the viability of a pregnancy but generally is not considered as reliable a marker as an HCG.
Imaging
An ultrasound correlated with a quantitative HCG can be diagnostic of ectopic pregnancy. An ectopic is suspected if the HCG is greater than 1500 and there is no evidence of an intrauterine gestational sac on transvaginal ultrasonography. On, intravaginal ultrasonography, an ectopic is suspected if an intrauterine pregnancy is not detected with a HCG level of greater than 6500.
| Right Sided Ectopic Pregnancy |
| 75763c02 75753c01 25 female positive HCG which doubled in 48 hours uterus showed prolifrative endometrium ovary right adnexa right ovary ectopic pregnancy position 2.5cms right ovarian cyst yolk sac gestational sac USscan Courtesy Ashley Davidoff MD |
| Empty uterus – No IUD, with Normal Left Ovary and Viable Adnexal Ectopic Pregnancy |
| 75791c01 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = no intraurterine pregnancy complex free fluid probably blood and hemorrhage b = normal left ovary c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01 |
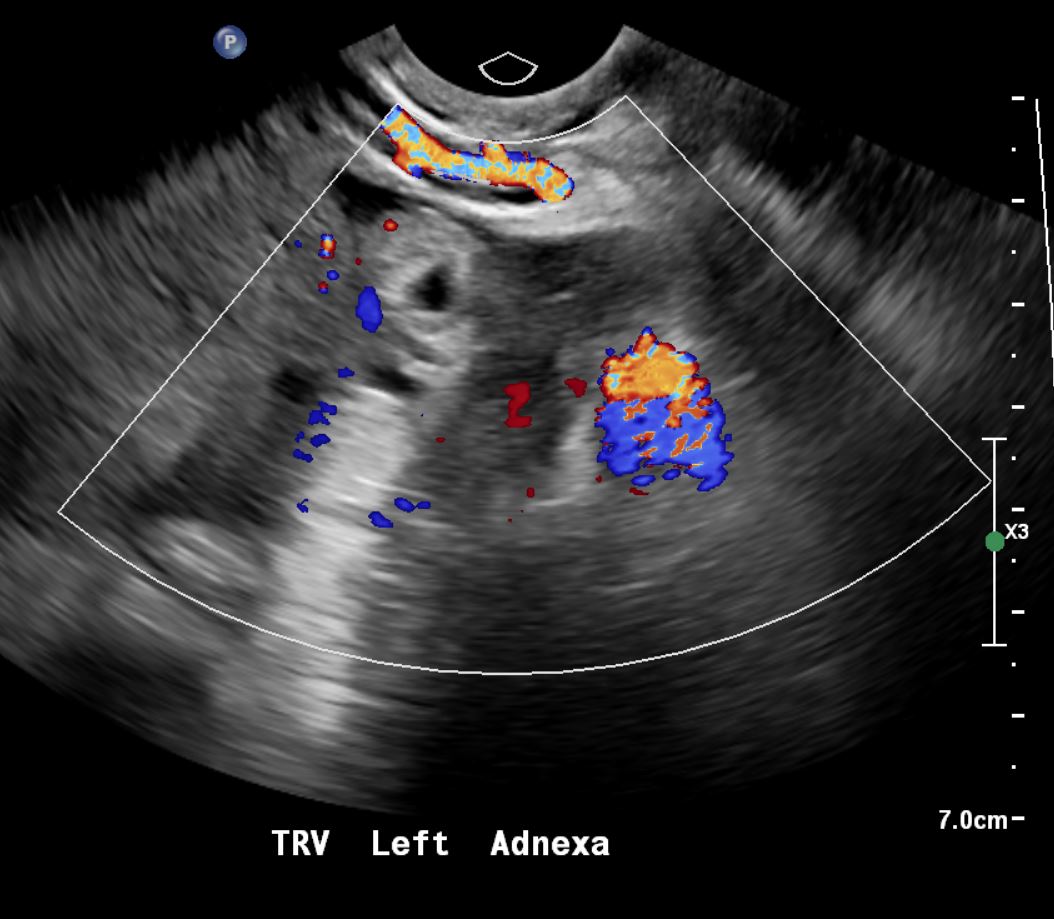
| Left Adnexal Ectopic Pregnancy with Hemorrhage |
| 75791c03 32 year old female presents with abdominal pain and pelvic pain positive HCG uterus endometrial stripe a = left ovary complex free fluid probably blood and hemorrhage b = left ovary complex free fluid probably blood and hemorrhage c = viable fetus in the left adnexa with fetal doppler flow heart beat d = crown rump length of .62cms corresponding to a gestational age of 6 weeks and 4 days dx left sided ectopic pregnancy US scan Courtesy Ashley Davidoff MD 75791 75791c01 75791c03 75792c01 |
Treatment and Management
There are several treatment options, and the appropriate selection depends on the clinical conditions. The options include expectant management, medical management, and surgical management. Expectant management: sometimes, if the pregnancy is early (with a serum HCG of < 1000 and declining) and the gestation is small (less than 3 cm), and absent fetal heartbeat, expectant management with close follow-up may be considered. If the patient is hemodynamically stable, it may be possible to treat the ectopic medically. Medical management typically involves methotrexate. Methotrexate is a chemotherapeutic agent which inhibits folate metabolism, therefore inhibiting the growth of rapidly dividing cells such as a new gestation. Surgical intervention typically involves laparoscopic surgery and most recently tubal incision to remove the gestation. Surgery is chosen for the unstable patient, larger, more advanced pregnancies, and for medical treatment failures.
| Occluded Left Fallopian Tube Following Ectopic Pregnancy |
| 75792c01 32 year old femalehistory of left sided ectopic pregnancy destruction and iatrogenic change in left Fallopian tube normal uterys normal right Fallopian tube spillage into the peritoneal cavity hysterosalpingogram Courtesy Ashley DAvidoff MD 75791 75791c01 75791c03 75792c01 |
Prognosis
Generally the prognosis of ectopic pregnancy is good if it is diagnosed in a timely fashion. However, this serious condition is also one of the most common causes of maternal death and infertility.
Conclusion
Ectopic pregnancy involves the abnormal location of a pregnancy, most commonly in a fallopian tube. Risk factors include those conditions which affect the structure and function of the fallopian tube including pelvic inflammatory disease, previous fallopian tube surgery, or previous ectopic pregnancy. Any woman with amenorrhea with a positive pregnancy test, pelvic or abdominal pain, and/or vaginal bleeding, needs to be evaluated for possible ectopic pregnancy. The gestation will not survive outside of the uterus. This potentially life threatening condition is treatable if diagnosed in a timely fashion. Potential complications of ectopic pregnancy include recurrent ectopic pregnancy, infertility, and death.
Cases


References
ANNE-MARIE LOZEAU, M.D., M.S., and BETH POTTER, M.D. “Diagnosis and Management of Ectopic Pregnancy,” American Family Physician, November 1, 2005: Volume 72/No. 9.
Vicken P Sepilian, MD, MMS, “Ectopic Pregnancy,” from Emedicine online; last edited August 17, 2007.
MCQ
- Ectopic pregnancies most commonly occur in the:
- Uterus
- Ovary
- Fallopian Tube
- Abdomen
- Classic symptoms of an ectopic pregnancy include all of the following except:
- Post-prandial right upper quadrant pain
- Vaginal Bleeding
- Pelvic pain
- Amenorrhea
- The preferred imaging technique for ectopic evaluation is:
- Plain Xrays
- Ultrasound
- MRI
- CT
- In a normal early pregnancy the HCG is expected to double every 24 hours (T/F)
- True
- False
- Potential complications of ectopic pregnancy include all of the following except:
- Recurrent ectopic pregnancy
- Anorexia
- Infertility
- Death
Answers: 1. c; 2. a; 3. b; 4. b; 5. b
