The Common Vein Copyright 2010
Introduction
Uterine structural changes are necessary to allow implantation, gestation and childbirth.
Early in pregnancy, the endometrium provides a suitable environment for implantation of the embryo. The abundant glands and stroma formed in the proliferative phase of the menstrual cycle provide a site for trophoblastic invasion. In the secretory phase these glands will also produce several products necessary for fertilization and implantation. The endometrial vascular proliferation of the secretory phase provides a rich blood supply for the embryo after implantation.
After implantation the muscle cells of the myometrium hypertrophy. This leads to an initial increase in the thickness of the uterine wall. However as the fetus grows, the uterine wall stretches and thins. The elastic and fibrous tissue content of the myometrium also increases. This allows the uterus to stretch and accommodate the growing fetus, placenta and amniotic fluid. By the end of pregnancy the uterus has increased in size 500 times. Vascular growth and vasodilation of the uterine vasculature increases blood flow to the uterus as the pregnancy progresses to provide fetal nourishment through the maternal-fetal circulation.
During labor the cervix undergoes important structural changes to allow delivery. Prostaglandins lead to increased enzymatic activity dissolving the cross-linking bonds between collagen fibers. This results in increased cervical elasticity, cervical effacement and cervical dilation. The pelvic outlet widens to allow the fetus to pass, a result of pelvic ligament stretching and relaxation. As the fetus passes into the birth canal, the uterus maintains contraction, transforming from a thin-walled organ with a large central cavity to a thick muscular organ with almost no space in the central cavity. During delivery, the muscles of the pelvic floor thin allowing the vaginal opening to stretch during childbirth. After delivery, constriction of the uterine vasculature decreases maternal blood loss.
|
Junctional Zone In Early Proliferative Phase |
|
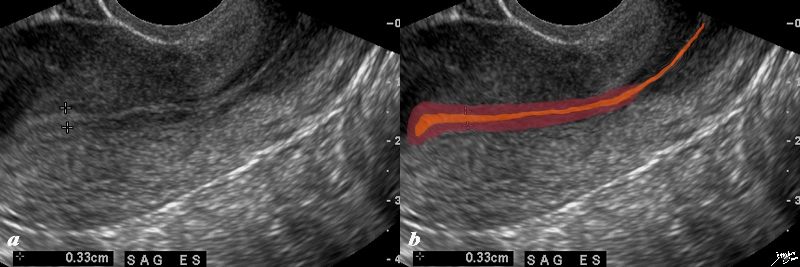
The normal sagittal view of the uterus is a transvaginal ultrasound, in the first week after menstruation after menstruation, and just prior to the next menstruation after the endometrium has been shed. It demonstrates that the endometrium becomes a single echogenic line consisting of opposing walls (orange) and is surrounded by a subendometrial halo of the junctional zone (tan). This layer is more compacted, and relatively hypovascular. This image is typical of the early proliferative phase. It is during this time that estrogen starts to rise and progesterone has fallen. The endometrium in this case measures about 3mms. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 84698c02b.8s |
|
Junctional Zone in the Premenstrual Uterus LMP 4 Weeks Prior |
|
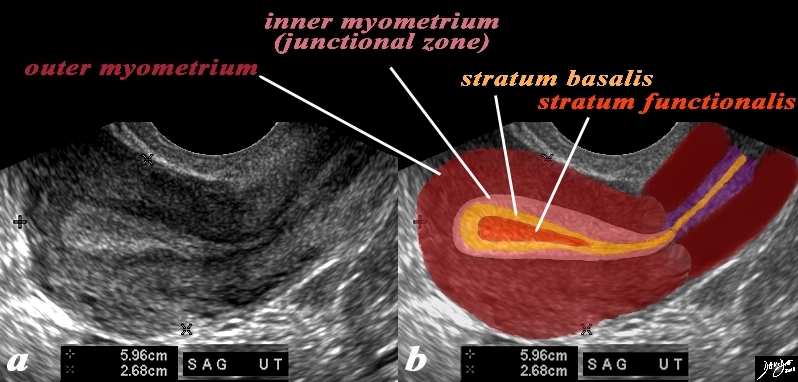
In this 26 year premenstrual female a transvaginal ultrasound in the sagittal plane reveals a normal view of the uterus with characteristic premenstrual appearance. (a) The stripe is almost homogeneously echogenic and thick but also shows a hypoechoic halo of the junctional zone or inner myometrium. (salmon) The homogeneous stripe is made up from two histological layers (barely distinguished by this ultrasound)– the inner stratum functionalis (deep orange) that will shed once the spiral arteries vasoconstrict, and the outer stratum basalis (deep yellow) that will not shed, and will be the basis for regenerating the endometrium in the next cycle. The next layer as stated above is the compact myometrium – the junctional zone (aka inner myometrium) , and is followed by the thicker outer myometrium (maroon). (b) Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 84538c06.83s |
Junctional Zone During Pregnancy
The junctional zone becomes disrupted increases in intensity and zonal differences become indistinct and returns to normal 6 months after deliver Willms AB Brown ED Keittritz UIRadiology 195 91-94 1995
|
Junctional Zone – Early Pregnancy |
|
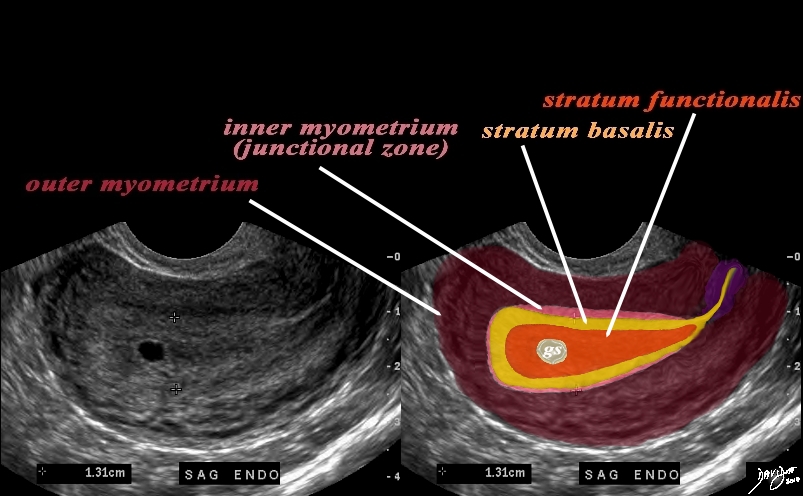
In this 16 year old patient her LMP was about 4 weeks ago and she had a positive pregnancy test. The transvaginal ultrasound in the sagittal plane reveals a normal view of the uterus with characteristic early pregnancy appearance characterized by the gestational sac (gs) embedded in the stratum functionalis (deep orange). The stratum basalis is seen as a slightly more echogenic layer around the functional layer (deep yellow). The stripe is thick measuring about The next layer is a barely seen junctional layer (salmon pink) best seen on the anterior subendometrial layer just beyond the basalis The next layer is the thicker outer myometrium (maroon) that contains dilated vessels. Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 84485c02.8ls |
|
|
Early in pregnancy, the endometrium provides a suitable environment for implantation of the embryo. The abundant glands and stroma formed in the proliferative phase of the menstrual cycle provide a site for trophoblastic invasion. In the secretory phase these glands will also produce several products necessary for fertilization and implantation. The endometrial vascular proliferation of the secretory phase provides a rich blood supply for the embryo after implantation.
After implantation the muscle cells of the myometrium hypertrophy. This leads to an initial increase in the thickness of the uterine wall. However as the fetus grows, the uterine wall stretches and thins. The elastic and fibrous tissue content of the myometrium also increases. This allows the uterus to stretch and accommodate the growing fetus, placenta and amniotic fluid. By the end of pregnancy the uterus has increased in size 500 times. Vascular growth and vasodilation of the uterine vasculature increases blood flow to the uterus as the pregnancy progresses to provide fetal nourishment through the maternal-fetal circulation.
During labor the cervix undergoes important structural changes to allow delivery. Prostaglandins lead to increased enzymatic activity dissolving the cross-linking bonds between collagen fibers. This results in increased cervical elasticity, cervical effacement and cervical dilation, allowing childbirth. After delivery, constriction of the uterine vasculature decreases maternal blood loss.
Structural Changes Non Gravid, 32 Week Pregnancy, and Post Cesarean Section |
|
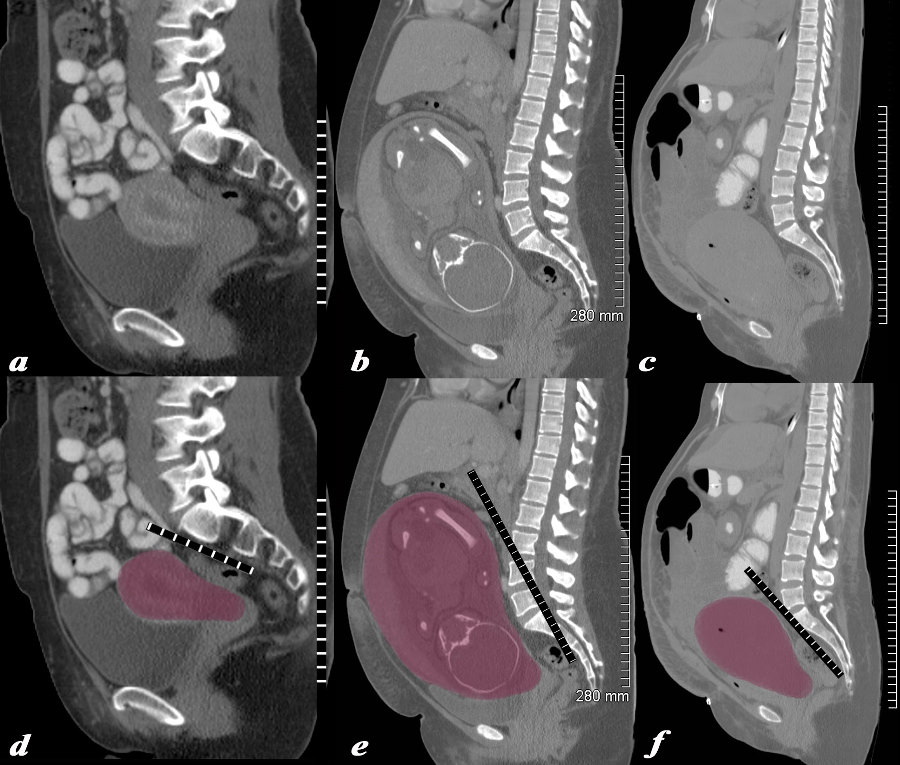
The series of CT scans from different patients are reconstructed in the sagittal plane to show the mature uterus in the non-gravid state (a,d) with a 32 week pregnancy (b,e), and in the postpartum, post cesarean section state (c,f). In the nongravid adult the uterus the craniocaudad span (c-c) measures about 9cms and the anteroposterior (A-P) dimension it measures 4.5cms The uterus containing the 32week pregnancy measures 24cms (c-c) by 16cms (A-P). In the post cesarean section patient the uterus measures 17cms (c-c) by 9cms (A-P). Courtesy Ashley Davidoff MD Copyright 2010 All rights reserved 78093c08.8s |
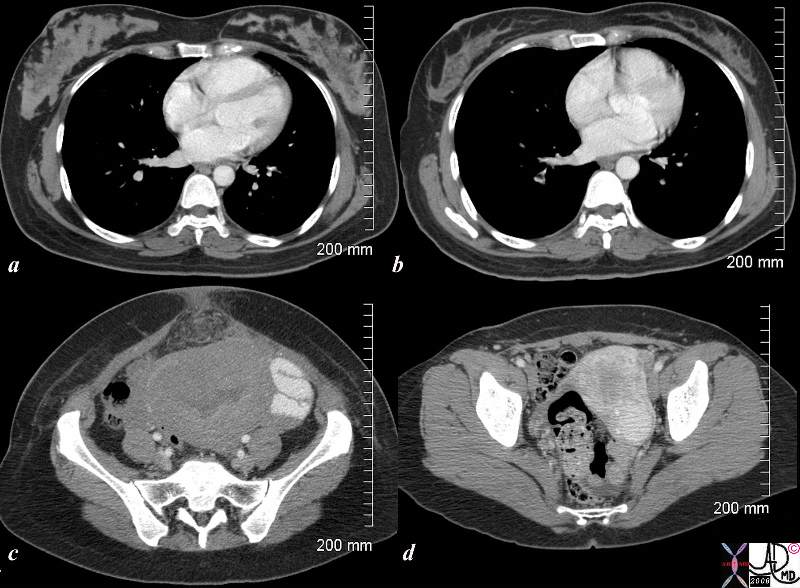
Postpartum and 18months Later |
|
The CTscan is from a 26 year old female showing breasts and uterus in a post partum post cesarian section state (a,c) and then 18months later (c,d). The transverse dimension of the uterus in the post partum state is about 11cms, while 18months later is about 5cms. Her breasts in the post partum state are enlarged with prominent glandular tissue (a), and in the post partum state are reduced in size and glandular volume (b). Surgical footprints are noted in the subcutaneous tissue in c following her cesarian section. A cervical fibroid is suggested post partum image (d). Courtesy Ashley Davidoff copyright 2009 83354c.8s |