Laura Miller MD Copyright 2010
Definition
Pelvic inflammatory disease (PID) is a sexually transmitted infection of the upper female genital tract.
The cause is usually polymicrobial and commonly includes Chlamydia trachomatis and/or Neisseria gonorrhea.
The result is chronic infection and inflammation leading to salpingitis, endometritis, and, in rare cases, tubo-ovarian abscess. The infection starts at the cervix and ascends to affect the endometrium and fallopian tubes.
The structural change in PID is minimal, though chronic inflammation from PID may cause adhesions of the fallopian tubes or peritoneal cavity.
The functional change is characterized by chronic infection and inflammation of the endometrium and fallopian tubes, predisposing women to infertility and ectopic pregnancy. Women usually present clinically with fever, vaginal discharge, pelvic pain and cervical motion tenderness on exam. In extreme cases, women with PID may present with septic shock.
Diagnosis is usually based on clinical presentation, though in some cases definitive diagnosis requires laparoscopy. Routine investigation of PID does not usually involve imaging. However, ultrasound is a useful diagnostic tool in women with suspected tubo-ovarian abscess.
Depending on the severity at presentation, treatment is with either oral or IV antibiotics. Empiric antibiotic coverage typically covers gonorrhea and chlamydia along with other common pathogens. (http://www.cdc.gov/std/treatment/2006/updated-regimens.htm) Most cases are treated as an outpatient. However, patients with more severe infection, abscess, uncertain diagnosis, pregnancy or immunosupression should be hospitalized for treatment.
Pelvic inflammatory disease (PID) is a sexually transmitted infection of the upper female genital tract which is usually caused by polymicrobial group that includes Chlamydia and/or Neisseria gonorrhea (GC) and results in salpingitis, endometritis, and may be complicated by tubo-ovarian abscess. The infection often starts at the cervix and travels upward. Possible complications include infertility and ectopic pregnancy.
The diagnosis usually rests on the clinical presentation includes fever, vaginal discharge, and pelvic pain and may be complicated by shock. Cervical tenderness is characteristic on examination. Imaging is not usually warranted unless a mass is felt on examination or the patient fails to improve on medical therapy.
Depending on the severity at presentation, treatment is with either oral or IV antibiotics. Management ideally is initiated even prior to results of cultures, which otherwise would delay treatment. A high index of suspicion is required and there are guidelines for empiric antibiotic coverage, typically to cover gonorrhea and Chlamydia along with other common pathogens. http://www.cdc.gov/std/treatment/2006/updated-regimens.htm. Those with mild to moderate symptoms may be treated with oral antibiotics unless there is concern they will be unable to complete this therapy, then they should be hospitalized. Patients with more severe infection, or abscess should be hospitalized for parenteral antibiotics. Likewise, if another serious etiology such as appendicitis can’t be excluded, the patient should be hospitalized.
Prevention includes routine screening for GC and Chlamydia for at risk groups.
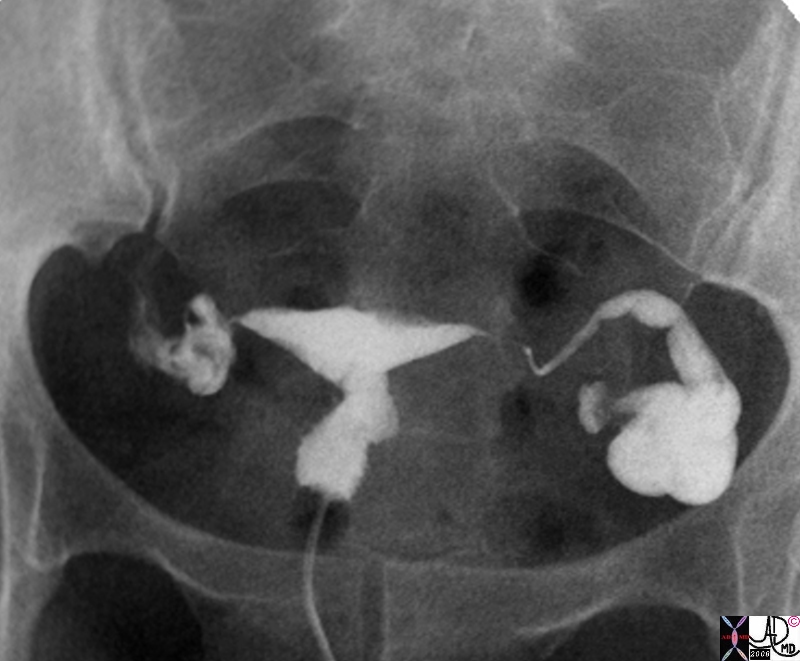
Obstructed Left Tube Hydrosalpinx |
| 33 old female with left adnexal discomfort and prior history of pelvic inflammatory disease Findings on hysterosalpingogram show a dilated fallopian tube consistent with hydrosalpinx uterus fallopian tube distended hydrosalpinx
83340b01.8s ultrasound USscan Courtesy Ashley Davidoff MD copyright 2009 |

Hydrosalpinx |
| 43 old female with right adnexal discomfort and prior history of pelvic inflammatory disease Findings on a transvaginal ultrasound show a dilated fallopian tube consistent with hydrosalpinx
uterus fallopian tube distended hydrosalpinx ultrasound USscan 83331.8s Courtesy Ashley Davidoff MD copyright 2009 |
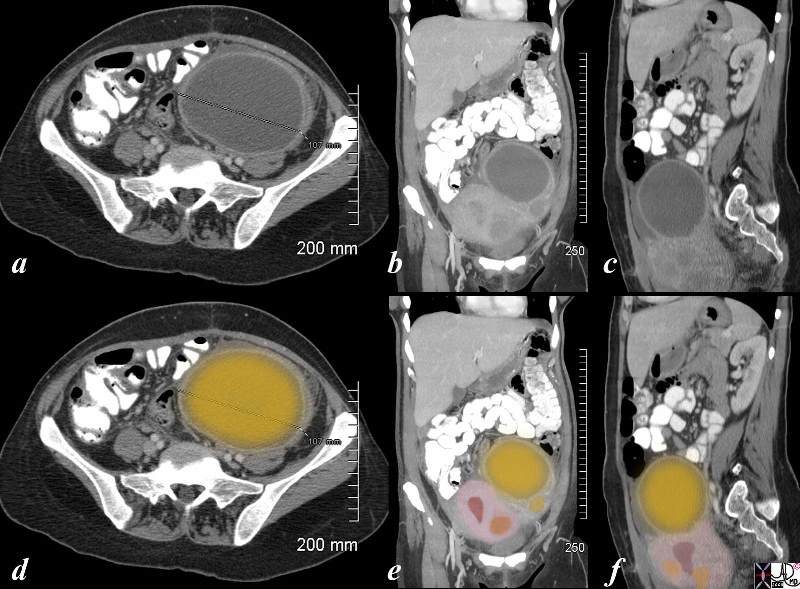
Left Ovarian Abscess |
| The CT is from a 36 year old female recently post cesarian section who developed pain the left lower quadrant, fever and rigors. She has a known fibroid uterus but a new tender mass was found in her left adnexa. The CTscan shows a large cystic collection in the left adnexa(dark yellow) with an enhancing rind. Pus was aspirated under ultrasound guidance , and a diagnosis of an ovarian abscess was made. She was treated on antibiotics and she subsequently her pain and fever resolved . The axial view (a,d) shows a 10.7 cms abscess. The coronal view (b,e) shows the large abscess in the left adnexa with a smaller abscess just below it (yellow) adnexa with the uterus and its endometrial cavity(maroon) and a fibroid in orange. The sagittal view (c,f) shows an irregular uterus (pink) with endometrial cavity (maroon) and a few fibroids (orange)
pain ovary PID pelvic inflammatory disease infection abscess CTscan Ashley DAvidoff MD copyright 2008 83287c03.8s |
